What to Expect at a DWI/DUI Assessment in New York
A DWI/DUI assessment at Spring Hill Wellness helps New Yorkers meet legal requirements and restore their license through confidential, OASAS-certified evaluations.

Understanding the Purpose of a DWI/DUI Assessment
After being charged with Driving While Intoxicated (DWI) or Driving Under the Influence (DUI) in New York State, one of the first legal steps is to complete an OASAS-approved Alcohol and Drug Assessment. This process, often referred to as a DWI evaluation, is part of the Impaired Driver System under New York State Vehicle and Traffic Law Section 1198-a (VTL 1198-a).
The goal is not to punish you — it’s to determine whether alcohol dependency or substance misuse contributed to the incident and to identify safe, appropriate next steps. Assessments are required for participation in the Impaired Driver Program (IDP), for reinstating a driver license or learner permit, or as part of sentencing under NYS DWI law VTL 1192.
At Spring Hill Wellness in Manhattan, our licensed counselors provide these OASAS-certified alcohol assessments confidentially and respectfully. We help clients meet legal requirements, satisfy court mandates, and move forward with confidence.
What Is an OASAS Alcohol Assessment?
An Alcohol Assessment — sometimes called an Impaired Driver Screening and Assessment — is a clinical evaluation performed by a licensed counselor or health-care provider certified by the Office of Addiction Services and Supports (OASAS).
The assessment follows strict assessment standards established by the Regulations of the Commissioner of Motor Vehicles and must comply with confidentiality laws (42 CFR Part 2) to protect your privacy. The outcome determines whether you’ll complete simple educational programming or enter a substance abuse counseling or rehabilitation program such as an Intensive Outpatient Program (IOP).
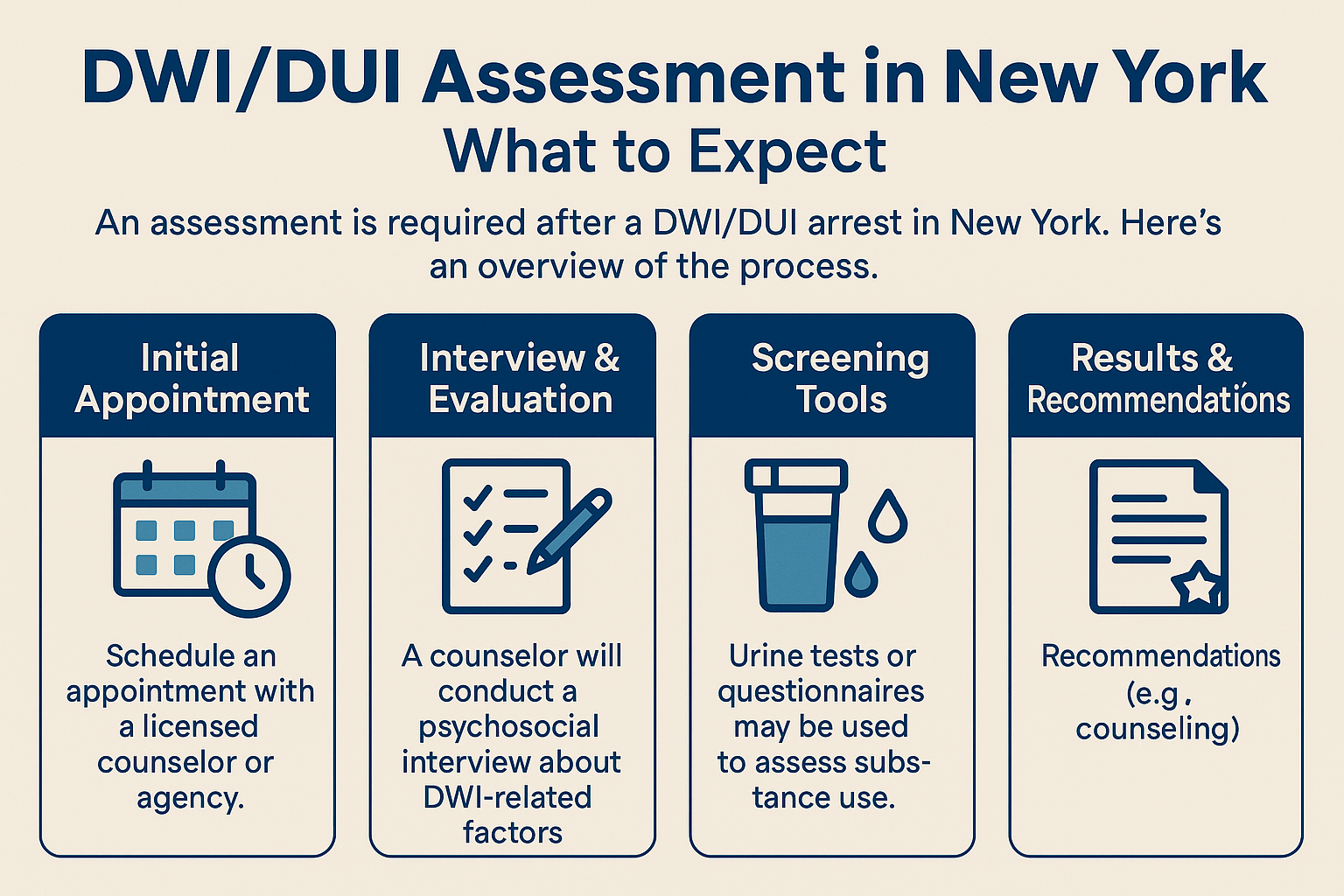
The DWI Evaluation Process
At Spring Hill Wellness, our DWI evaluation process is designed to be straightforward and supportive. A typical session lasts about 60 to 90 minutes and includes:
- Intake Appointment & Psychosocial Interview – A licensed clinician reviews your personal history, lifestyle, hobbies, social life, and physical and mental health.
- Review of Legal Documents – We look over your police report, breathalyzer tests, and any field sobriety test details or probable-cause documentation provided by the New York State Trooper or local law enforcement.
- Substance-Use Screening – You may complete standardized questionnaires and a urine drug screening or chemical test to measure blood-alcohol concentration (BAC).
- Evidence-Based Assessment & Clinical Review – The clinician uses time-tested assessment tools to evaluate risk levels and determine whether substance use education or treatment is necessary.
- Evaluation Report & Recommendations – You receive a written summary suitable for your court process, criminal defense attorney, or Driver Improvement Unit, including whether treatment options or continued monitoring are recommended.
This process aligns with Part 136.1 (b)(3) of the NYS DMV Regulations, ensuring every assessment meets state requirements for accuracy and fairness.
Required Documentation and Forms
Before your appointment, you’ll need:
- Valid driver license or photo ID
- Police Report or breathalyzer report from the arresting agency
- Any court or probation paperwork
- The DS-449 Form (official OASAS Drug and Alcohol Assessment Referral)
- Insurance or payment information
If your assessment is court-ordered in Suffolk County or the Hudson Valley, results are automatically shared with the appropriate Driver Improvement Unit or court clerk, helping to streamline the license restoration process.
What Questions Will They Ask?
Clients often worry about what happens in the room. The psychosocial interview covers:
- Your alcohol or drug-use history
- Medical records, medication use, and physical health
- Family history and mental health background
- Daily routines, stressors, and coping strategies
- Attitudes toward alcohol and safe driving
Your counselor may ask about the traffic stop, breathalyzer results, or use of an ignition interlock device if applicable. Remember, the conversation is confidential and focused on creating a plan that satisfies the legal system and supports your recovery.
How Long Does a DWI/DUI Assessment Take?
The entire appointment typically lasts about 90 minutes. Some evaluations require an additional follow-up or verification session if documents are incomplete. Clients who prefer convenience can choose virtual assessments through secure, HIPAA-compliant telehealth platforms.
If Treatment or Education Is Recommended
Depending on your results, you may be referred to:
- The Impaired Driver Program (IDP) or Drinking Driver Program for education
- An Outpatient Counseling or Rehabilitation Center such as Spring Hill Wellness
- Alcoholics Anonymous or Narcotics Anonymous meetings for peer support
- A DOT Substance Abuse Professional (DOT/SAP) Evaluation if you hold a commercial driver license
Our team can also help coordinate Medication-Assisted Treatment, ongoing Substance Abuse Counseling, or alcohol rehabilitation programs to satisfy both OASAS and DMV requirements.
How Spring Hill Wellness Helps New Yorkers
Spring Hill Wellness, located in Manhattan, is fully OASAS-certified to perform DWI/DUI alcohol evaluations throughout New York City and New York State. Our licensed clinicians provide a non-judgmental environment, using evidence-based assessments and a clinical assessment process that meets every assessment standard required by law.
We also handle coordination with attorneys, courts, and probation officers so your evaluation report and Letters of Recommendation reach the proper agencies promptly. Clients across Brooklyn, Queens, The Bronx, Hudson Valley, and Long Island rely on us for fast, confidential assessments and clear next steps toward license restoration and compliance.
Taking the Next Step
Completing your DWI/DUI Alcohol Assessment is an important step toward regaining your driving privileges and rebuilding peace of mind. Whether you were referred after a traffic stop, a court hearing, or as part of a DOT/SAP evaluation, our team is here to help you navigate the process with care and professionalism.
Contact Spring Hill Wellness today to schedule your OASAS-approved Alcohol Assessment — available in person or online — and take the first step toward getting your license restored and your life back on track.




